Saturday, February 11, 2006
Tight Brain Checklist
-
Printer Friendly|#| Trackback
The anesthetist can have a significant impact on the operating conditions a neurosurgeon has to work with. One example is a situation where the surgeon (or anesthetist) notices the brain no longer appears relaxed but begins to get 'tight' within the craniotomy window. Rather that a knee-jerk response of further hyperventilating the patient and/or giving Mannitol, it is prudent to first consider possible causes as follows:
- Are the pressures controlled?
- Is the metabolic rate controlled?
- Are vasodilators in use?
- Are there any unexpected mass lesions?
Are the pressures controlled?
- Arterial Pressure
- pCO2
- pO2 (remember that hypoxemia is a potent stimulus for cerebral vasodilation
- Intrathoracic pressure
- Airway pressure
- Jugular venous pressure (includes external venous compression by C-spine collar or twill used to secure endotracheal tube)
Is the metabolic rate controlled?
- Pain
- Light anesthesia
- Awareness
- Seizures
Are vasodilators in use?
- Potent agents (Isoflurane, Desflurane, Sevoflurane, Enflurane)
- Nitroprusside
- Nitroglycerine
Are there any unexpected mass lesions?
- Pre-existing pneumocephalus exacerbated by nitrous oxide
- Cerebral hemorrhage remote to the site of surgery
As taught to me by John Drummond, M.D. at UCSD
Wednesday, February 1, 2006
Pandora's Box Of Music
-
Printer Friendly|#| Trackback
It looks to me like this would solve the OR's music problems. Staff could pre-program their favorite station and just log in from an operating room computer...as long as that wouldn't interfere with online shopping...
Friday, November 25, 2005
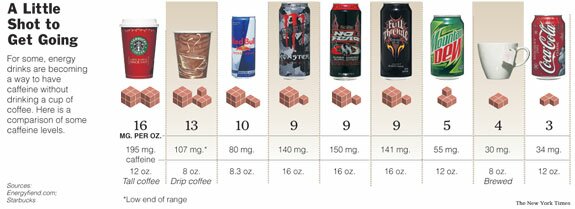
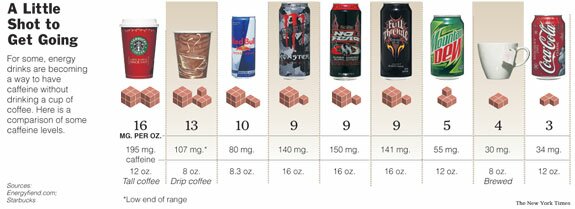
How much caffeine does that drink have?
-
Printer Friendly|#| Trackback
I've written before about caffeine addiction in surgical patients. In recent years there's been an explosion of caffeine-containing beverages. Having some idea of the caffeine content of the major ones can help you choose an appropriate dose.
The Energy Fiend web site has a nice Caffeine Database. I found it via a recent NYT article.
Thursday, November 24, 2005
How To: Awake Fiberoptic Intubation
-
Printer Friendly|#| Trackback
This definitely falls in the "don't try this at home" category, but if this technique is different than the one you use, give it a try. It will surely result in a net gain in style points.
How To Do An Awake Fiberoptic Intubation
Technorati Tags: Anesthesia
Sunday, November 20, 2005
More on pre-emptive positioning
-
Printer Friendly|#| Trackback
A fellow anesthesiologist wrote a reply to my post about pre-emptive positioning with the following:
"We've started doing the same thing at my surgicenter. At first I thought it was pretty ballsy when one of my colleagues suggested that we do simple one level laminectomies under LMA general and induce in the prone position. But now that we've started it I am very comfortable with the idea."
I'm not ready to try this yet (do you want to be my first patient?). Lateral or semi-sitting to supine is a matter of seconds. Prone to supine would take significantly longer I believe. Other experiences?
Sunday, November 6, 2005
You Anesthesiologist Today Was...
-
Printer Friendly|#| Trackback
I finally ordered my own business cards. I've had generic one available but always had to write in my own name (despite being with the group for well over two years) so decided it was time for an upgrade.
Picking the pattern was tough, but I decided on a tranquil image (that happens to be one of the MacOS X desktop images):
Rejected images included a dark tunnel with a light at the end, and anything with pearly gates.
This decision was evidence based (of course). Giving patients a business card before anesthesia increases their recall of your name to about 50% rather than the 10% that remember it without. It should also help them see they are being cared for by a physician. There's room on the back for 'anesthetic' and 'comments', too.
Thursday, November 3, 2005
Pre-emptive Patient Positioning
-
Printer Friendly|#| Trackback
Many surgeries require the patient to be in a position other than supine (flat on their back) for the surgery to be done. Shoulder surgery, for example, is often done with the patient in a semi-sitting or 'beach chair' position. Certain hip surgeries are done with patients on their side as well. General anesthesia is induced with the patient supine, then people have to move the patient (who is now akin to a very heavy sack of potatoes) into the right position. It's time consuming, risks staff injury, and jeopardizes the airway. The few accidental extubations I've had have occurred when the patient was being moved. Does it have to be this way? If the case is amenable to an LMA, I think the answer is 'no.'
If I'm caring for a patient who will require a general anesthetic and an LMA would be suitable, I've taken to positioning the patient before induction of anesthesia. I then pre-oxygenate, perform an IV induction, and place the LMA. The OR staff and surgeons like it because a) it saves time and b) it saves their backs. I like it because there's no move during which my airway can potentially be compromised (and because it saves time and saves my back). There's a benefit to the patient, too. Namely, they can tell us while awake whether our positioning is comfortable for them. Is the axillary role in the right place? Do they need a pillow under their knees in? Is their bottom up against the back of the table in beach chair? Is their ear properly padded in the lateral position? Think Different (but always, Think Safe).
Saturday, April 23, 2005
When can nursing mothers resume breastfeeding after surgery?
-
Printer Friendly|#| Trackback
When can nursing mothers resume breastfeeding after surgery?:
" the very small amount of propofol eliminated in breast milk within the first 24 hours after induction of anesthesia represents such minimal infant exposure to the drug that it provides insufficient justification for interruption of breastfeeding, Avram said. "
Studies are under way by the same group for other commonly used drugs. My advice to nursing patients is to pump and discard once, then resume normal breast feeding.
Friday, January 21, 2005
Why I Like Being An Anesthesiologist
-
Printer Friendly|#| Trackback
I've tried to explain to people why I like being an anesthesiologist so much--with difficulty (unfettered access to narcotics, starting my work day at 07:30, having patients ask me if I'm a real doctor, oodels of respect from surgeons and nurses alike are the reasons that usually come to mind). I just ran across something on the web that really helps me understand why. Getting Back To Work: A Personal Productivity Toolkit at kuro5hin.org is an article about procrastination. Now, my favorite motto is 'hard work pays off after a time, but laziness pays off now,' so I was naturally drawn to this article.
The article describes the ideal work experience as being in a state of 'flow' and goes on to outline the kinds of tasks that make it more likely you'll be able to attain it:
"
- Variety
- Appropriate and flexible challenges
- Clear goals
- Immediate feedback
- A sense that one's skills are adequate to cope with the challenges at hand.
- A rule-bound action system
This is what the ideal job looks like. This job will resemble play, and will be addictive. As much as you can create work like this, you will be a happy person. As much as you can make your work like this, you will want to do it. "
Bingo! That's why I like being an anesthesiologist in private practice!
That's also why I like using Conversant to build web sites. When I'm working on a Conversant site, I often reach a state of 'flow.'
[Via 43 Folders]
Wednesday, January 12, 2005
Triple Lumen Catheters Are Not Volume Lines
-
Printer Friendly|#| Trackback
I brought a patient to the operating room recently who had a Type A ascending thoracic aneurysm dissection. She was bleeding into her pericardium and was in tamponade on arrival. She had a radial arterial line that wasn't (in an artery), and two triple lumen central lines--one in a femoral vein and one in an internal jugular vein.
I immediately thought back to my medical school days when I would see patients in the ICU with a GI bleed being transfused with cold, undiluted packed red blood cells through a triple lumen central line....and they were on vasoactive drips for 'hypotension.'
What's my point? Triple lumen catheters are long and narrow (especially compared to Cordis introducer sheaths or products like them made by other manufacturers such as Arrow). Remember the Poiseuille-Hagen equation shows that flow rate is directly proportional to the fourth power of the radius, to the viscosity of the fluid being transfused, and to the pressure gradient established and inversely proportional to the length of the tube. A 9 French introducer sheath can infuse fluid at about 1000 cc/min. Compare that to about 250 cc/min for the 14 gauge lumen of a triple lumen catheter. So it follows, then, that if you need to give someone fluid (like blood) fast, you infuse it through a fat catheter that is short, reduce the viscosity by diluting it and warming it (in the case of packed red blood cells), and apply some pressure by elevating it well above the patient or putting a pressure bag on it. Got it? Good! This might come in handy when you next see a hypovolemic patient...
| |
1
|
2 |
3 |
4 |
| 5 |
6 |
7 |
8 |
9 |
10 |
11 |
| 12 |
13 |
14 |
15 |
16 |
17 |
18 |
|
19
|
20 |
21 |
22 |
23 |
24 |
25 |
| 26 |
27 |
28 |
|
|
Nov Feb
|