Friday, June 9, 2006
Two Google Firefox Extension: Browser Sync and Notebook
-
Printer Friendly|#| Trackback
Let's say you're like me use hospital computers a great deal. There are some neat tools you should know about to make hospital computers feel more like home. Here are my suggestions:
1. Use a USB thumb drive and install Portable Firefox.
Every hospital computer I've ever used has Internet Explorer as the default browser (sigh). Most don't allow you to install your own software. Having a USB thumb drive with your own lean, mean, pop-up blocking copy of Firefox gives you the browser preferred by nine out of ten dweebs. Any extensions you install are on the USB drive and travel with you. Lifehacker has a nice article on this. Speaking of extensions...
2. If you haven't already done so, get a Google account.
3. Install the Google Browser Sync Extension for Firefox.
I may get around when it comes to using lots of computers, but I do have a first love--my Apple MacBook. (The mooing sounds it makes are just so endearing). And that's where I spend most of my computer time and subsequently have the best organized set of bookmarks. The Browser Sync Extension synchronizes bookmarks, history, persistent cookies, and saved passwords between computers. For more on the security implications, see Lifehacker...
4. Install the Google Notebook Extension for Firefox.
I will occasionally find web content when I'm at the hospital that I want to look at when I get back home. The Notebook extension adds an additional contextual menu option to 'Note This...' which adds the page title, URL, and selected text to my Google Notebook where I can read it later.
5. Set up your Google Home Page and add the Body Mass Index and Allowable Blood Loss modules!
Sunday, June 4, 2006
NEJM CME: Body-Mass Index and Symptoms of Gastroesophageal Reflux in Women
-
Printer Friendly|#| Trackback
CME: Body-Mass Index and Symptoms of Gastroesophageal Reflux in Women
"Conclusions: BMI is associated with symptoms of gastroesophagealreflux disease in both normal-weight and overweight women. Even moderate weight gain among persons of normal weight may cause or exacerbate symptoms of reflux."
Thursday, May 25, 2006
Top 10 Causes of Death Worldwide
-
Printer Friendly|#| Trackback
Top 10 Causes of Death Worldwide:
"[F]or high-income countries:
1. Heart disease
2. Stroke
3. Lung cancer
4. Lower respiratory infections
5. Chronic obstructive pulmonary disease (COPD)
6. Colon and rectum cancers
7. Alzheimer's disease and other dementias
8. Type 2 diabetes
9. Breast cancer
10. Stomach cancer
Here is the list for low- and middle-income countries:
1. Heart disease
2. Stroke
3. Lower respiratory infections
4. HIV/AIDS
5. Fetus/newborn (perinatal) conditions
6. Chronic obstructive pulmonary disease (COPD)
7. Diarrhea
8. Tuberculosis
9. Malaria
10. Road traffic accidents "
[Via WebMD Health Headlines]
Wednesday, May 24, 2006
Pennsylvania's Health Care Crisis has NOT 'turned the corner'
-
Printer Friendly|#| Trackback
Our Governor is quoted as saying that Pennsylvania's health care crisis has turned a corner. It has not and as evidence I point you to the following article about a Cardiology group in Philadelphia that will no longer provide coverage at one health center there:
"Frankford Health Care System, which is already getting ready to discontinue maternity services at its Torresdale division, is losing another group of specialists at its Frankford campus in another departure tied in part to Pennsylvania's high medical malpractice insurance costs. --Philadelphia Business Journal"
Imagine you're, say, a plastic surgeon. There used to be fifteen of you on staff at a hospital so you took ER call only two days per months (as a precondition for maintaining staff privileges). Well, because of a malpractice crisis that has NOT turned the corner there are only three of you now. That's ten days of ER call each month. Kinda forces you to ponder whether maintaining staff privileges is worth is, doesn't it? And if you decide it's not, then patients loose access to yet another specialist at the hospital. See where this goes?
If it's not one virus, it's another
-
Printer Friendly|#| Trackback
Bird flu has been very much in the news, but now another type of virus is also threatening: chikungunya virus (named with a Swahili word meaning 'bent up').
"The chikungunya virus has infected around one-third of the population (about 250,000 people) on the French island of Réunion since early 2005. It has also hit the neighbouring islands of Mauritius, Seychelles, Madagascar and Mayotte, and reared its head in India."
With only a little over 200 deaths it's not near as big a killer as H5N1 might be, but it would wreak havoc nonetheless. Fevers over 102 and arthralgias. Yuck.
Sunday, May 14, 2006
RangelMD on Tort Reform in Texas
-
Printer Friendly|#| Trackback
Texas enacted caps on medical malpractice awards in 2003. The debate there on whether these caps are good or have been responsible for the drop in new malpractice cases by 60%-80% continues.
"Obviously the need is to reduce legal costs, increase ease and access to the system, increase efficiency and speed of proceedings so that justified compensation finds its way to the plaintiff with all deliberate speed, and establish much more consistency in finding fault and awarding compensation. One solution is the establishment of special health courts where neutral expert witnesses would be hired by the court, judges or panels would hand down judgments, and guidelines would be in place for the determining of fault and compensation.
It's easy to see why trial lawyers oppose special health courts because their roles would be significantly reduced. A system like this would be far less susceptible to such intangibles as the fickle mood of a jury or the charisma of the lawyer. We've been talking for years about reducing costs and improving access to health care. Maybe it's about time we started doing the same with our tort system. Proposition 12 may have been the first small step in that direction."
[RangelMD]
Friday, May 12, 2006
Wet taps and the number '3'
-
Printer Friendly|#| Trackback
Wet taps are accidental dural punctures that happen while attempting to place a needle into the epidural space. The published frequency of wet taps is about 1 in 800 epidural placements, depending on the experience of the operator. If I'm placing an epidural catheter in a pregnant woman and get a wet tap, she has a greater than 50% chance of a dural puncture headache (unless, of course, she is morbidly obese, in which her risk is almost zero).
It seems my wet taps come in three's (hence the title of this post). I remember as a third year anesthesiology resident being on call on OB for the first time after spending three months on the transplant anesthesia service and getting three consecutive wet taps that night on OB. Bam, bam, bam (or should I say 'splash, splash, splash'). I felt terrible, of course, but could not recall doing anything different that would have caused them! My grandmother used to say that accidents happen in threes. She was referring to airplane crashes, but I have to wonder, is it true of wet taps?
In the last ten years of doing anesthesia I've had no accidental dural punctures that I know of. That all changed about a month ago. I did a lumbar epidural steroid injection on a co-worker's husband and must have scored the dura. That's one. I had a wet tap during a labor epidural on a patient who, in retrospect, had a non-union of the ligamentum flavum. That's two. I'm just waiting for number three. I'm on call on OB tonight. Is number three around the corner?
[here's a nice review, btw]
Tuesday, May 2, 2006
Don't Touch My Oxygen!
-
Printer Friendly|#| Trackback
Most days are nice. Occasionally I get into a head-butting contest with a nurse or surgeon (but much less often than when I was younger). Of late, it seems to be an almost daily occurrence. Today's example? I arrived at a surgery center to start cases to find the oxygen failure alarm triggered on all our anesthesia machines. After telling colleagues and putting all rooms on hold, I figure out that a valve leak the day before had required a valve to be removed and the resulting system did not have enough oxygen pressure to keep the alarms from triggering. This was fixed in about 15 minutes and we proceeded.
Several hours later a nurse manager told me they were going to switch the oxygen system back to the way it was. I told her that, in my opinion, this should not be done until all cases for the day were finished. 'But it will only take a minute' was her reply. I told here once more that in my opinion as an anesthesiologist, no one should mess with a system that was presently working and that the safest thing to do was wait until rooms were down. She left and had the technicians make the switch.
She will now learn the hard way that you do not touch my oxygen while cases are under way. When it comes to patient safety, our opinions are not equal...
VeinViewer
-
Printer Friendly|#| Trackback
"
VeinViewer Shipped!

"The VeinViewer, a device that reveals the underlying venous anatomy for easy IV placement, is now being shipped, according to RedHerring.com....Note to nurses on the floor: call VeinViewer and not an on-call anesthesiologist.
Company website | Video of VeinViewer
"
[Via Medgadget]
Friday, April 21, 2006
Archives of Surgery: Incidence, Patterns, and Prevention of Wrong-Site Surgery
-
Printer Friendly|#| Trackback
Incidence, Patterns, and Prevention of Wrong-Site Surgery [free]
"Results Among 2 826 367 operations at insured institutions during the study period, 25 nonspine wrong-site operations were identified, producing an incidence of 1 in 112 994 operations (95% confidence interval, 1 in 76 336 to 1 in 174 825). Medical records were available for review in 13 cases. Among reviewed claims, patient injury was permanent-significant in 1, temporary-major in 2, and temporary-minor or temporary-insignificant in 10. Under optimal conditions, the Joint Commission on Accreditation of Healthcare Organizations Universal Protocol might have prevented 8 (62%) of 13 cases. Hospital protocol design varied significantly. The protocols mandated 2 to 4 personnel to perform 12 separate operative-site checks on average (range, 5-20). Five protocols required site marking in cases that involved nonmidline organs or structures; 6 required it in all cases."
The facilities I work at use 'Time Out' and are gradually standardizing on the use of the word 'yes' to mark the site (which I believe to be the best). Administrators tend to add things to the Time Out so they can say they did something about a problem. Our time outs now require confirmation of a negative pregnancy test before GYN surgery as well as 'Implants Available' for cases that will use implants; a list which will no doubt get longer as more errors occur.
The article contains this jewel from a well known author on errors in medicine--James Reason:
"First, written checklists, although designed for easy use, are prone to several types of error: skipped steps due to interruptions and distractions and stating that an item has been completed (checking the box) when in fact it has not. Second, redundant checks can achieve an exponential decrease in risk of error but only if each checkpoint is independent. Third, increasing the number of involved caregivers can foster routine violations because the multiple checks begin to seem like "busy work." Finally, efforts to keep up with the pace of patient flow may lead to viewing violations of protocol as acceptable or necessary. Simplification of protocols would improve adherence and efficiency and allow surgical teams to focus their limited time and energy on prevention of more common or harmful errors."
Thursday, April 20, 2006
Identity Theft Disclosure Law: Congress About To Fail Us Again
-
Printer Friendly|#| Trackback
Bruce Schneier, in Identity-Theft Disclosure Laws explains why pending federal legislation on protecting consumers form identity theft is a step backward from many existing state laws.
"...this federal law pre-empts the 23 existing state laws -- and others being considered -- many of which contain stronger individual protections. So while [the Data Accountability and Trust Act] might look like a law protecting consumers nationwide, it is actually a law protecting companies with large databases from state laws protecting consumers.
So in its current form, this legislation would make things worse, not better."
Tuesday, April 11, 2006
Two New Google Modules
-
Printer Friendly|#| Trackback
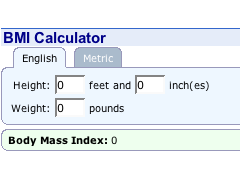
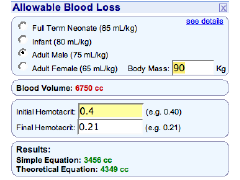
Seth Dillingham and I have created two modules for the Google personalized home page : Allowable Blood Loss and BMI Calculator. Despite having been submitted a week ago they are still not included in their directory, but I thought it safe to post about them here....
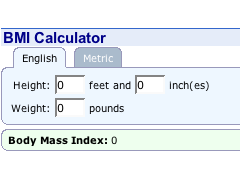 |
BMI calculates the Body Mass Index using the US or metric system. Furthermore, it can be used to convert from one system to the other.

|
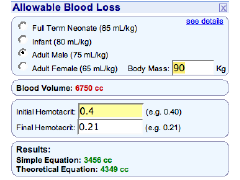 |
The Allowable Blood Loss Calculator gives a fairly good estimate of how much blood a patient would have to lose to cause a drop in hematrocrit to a specified amount assuming euvolemia is maintained.

|
Pet Peave: popular press articles that don't link to their sources
-
Printer Friendly|#| Trackback
The New York Times Online has an article titled 'Blasting of Kidney Stones Has Risks, Study Reports'. The article mentions the journal (The Journal of Urology) and the first author (Dr. Amy Krambeck). Would it have been so difficult to link to the abstract in the online version?
" SWL has revolutionized the management of nephrolithiasis and it is a preferred treatment for uncomplicated renal and proximal ureteral calculi. Since its introduction in 1982, conflicting reports of early adverse effects have been published. However, to our knowledge the long-term medical effects associated with SWL are unknown. We evaluated these adverse medical effects associated with SWL for renal and proximal ureteral stones.
Materials and Methods
Chart review identified 630 patients treated with SWL at our institution in 1985. Questionnaires were sent to 578 patients who were alive in 2004. The response rate was 58.9%. Respondents were matched by age, sex and year of presentation to a cohort of patients with nephrolithiasis who were treated nonsurgically.
Results
At 19 years of followup hypertension was more prevalent in the SWL group (OR 1.47, 95% CI 1.03, 2.10, p = 0.034). The development of hypertension was related to bilateral treatment (p = 0.033). In the SWL group diabetes mellitus developed in 16.8% of patients. Patients treated with SWL were more likely to have diabetes mellitus than controls (OR 3.23, 95% CI 1.73 to 6.02, p <0.001). Multivariate analysis controlling for change in body mass index showed a persistent risk of diabetes mellitus in the SWL group (OR 3.75, 95% CI 1.56 to 9.02, p = 0.003). Diabetes mellitus was related to the number of administered shocks and treatment intensity (p = 0.005 and 0.007).
Conclusions
At 19 years of followup SWL for renal and proximal ureteral stones was associated with the development of hypertension and diabetes mellitus. The incidence of these conditions was significantly higher than in a cohort of conservatively treated patients with nephrolithiasis. "
Before people panic (or call lawyers), please consider that this is one study, retrospective, with a 59% response rate, using older lithotripsy technology (as the NYT article points out, modern machines use less energy and are able to focus it more precisely.
| |
1 |
2 |
3 |
|
4
|
5 |
6 |
7 |
8 |
9 |
10 |
|
11
|
12 |
13 |
14 |
15 |
16 |
17 |
| 18 |
19 |
20 |
21 |
22 |
23 |
24 |
| 25 |
26 |
27 |
28 |
29 |
30 |
|
|
May Jul
|