Nothing can stand between me and my bluegrass
-
Printer Friendly|#| Trackback
On call at the hospital today. The work is done and we're getting ready to order Chinese food. Time for some computer work and bluegrass. But wait! The hospital has decided to block XM streams!
Thank you iTunes: Bluegrass Radio 128 kbps 100 Percent Pure Acoustic Bluegrass
Life is good (again).
Safety Tip: Nerve Block Needle Disposal
-
Printer Friendly|#| Trackback
I most commonly use a 2 inch B-bevel insulated needle for nerve blocks. It is often not convenient to dispose of the block needle right away after completing the block, so I started placing it in the barrel of the empty syringe from the plunger side and holding it in place with by depressing the plunger. Like this:

Safer for myself and my assistant (when I have an assistant).
YouTube: Site-Rite Instructional Video
-
Printer Friendly|#| Trackback
The AHRQ published Making Health Care Safer: A Critical Analysis of Patient Safety Practices in 2001. Chapter 21 deals with Ultrasound Guidance of Central Vein Catheterization. I thought I'd include a link to a YouTube video that shows how this device is used:
Although the device has advance considerably since then (see below), the images it provides are still pretty much the same.
I will often use the device to locate and mark an internal jugular vein before draping the patient as I find the use of the needle guide extremely cumbersome.
[Site-Rite]
Tight Brain Checklist
-
Printer Friendly|#| Trackback
The anesthetist can have a significant impact on the operating conditions a neurosurgeon has to work with. One example is a situation where the surgeon (or anesthetist) notices the brain no longer appears relaxed but begins to get 'tight' within the craniotomy window. Rather that a knee-jerk response of further hyperventilating the patient and/or giving Mannitol, it is prudent to first consider possible causes as follows:
- Are the pressures controlled?
- Is the metabolic rate controlled?
- Are vasodilators in use?
- Are there any unexpected mass lesions?
Are the pressures controlled?
- Arterial Pressure
- pCO2
- pO2 (remember that hypoxemia is a potent stimulus for cerebral vasodilation
- Intrathoracic pressure
- Airway pressure
- Jugular venous pressure (includes external venous compression by C-spine collar or twill used to secure endotracheal tube)
Is the metabolic rate controlled?
- Pain
- Light anesthesia
- Awareness
- Seizures
Are vasodilators in use?
- Potent agents (Isoflurane, Desflurane, Sevoflurane, Enflurane)
- Nitroprusside
- Nitroglycerine
Are there any unexpected mass lesions?
- Pre-existing pneumocephalus exacerbated by nitrous oxide
- Cerebral hemorrhage remote to the site of surgery
As taught to me by John Drummond, M.D. at UCSD
Pandora's Box Of Music
-
Printer Friendly|#| Trackback
It looks to me like this would solve the OR's music problems. Staff could pre-program their favorite station and just log in from an operating room computer...as long as that wouldn't interfere with online shopping...
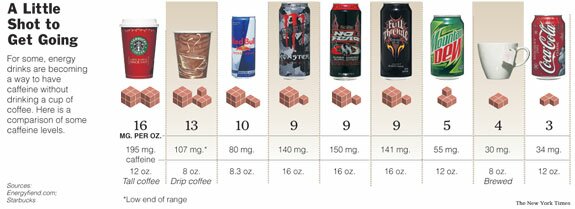
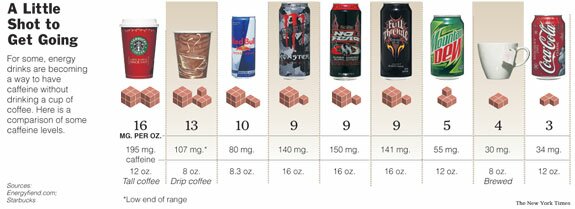
How much caffeine does that drink have?
-
Printer Friendly|#| Trackback
I've written before about caffeine addiction in surgical patients. In recent years there's been an explosion of caffeine-containing beverages. Having some idea of the caffeine content of the major ones can help you choose an appropriate dose.
The Energy Fiend web site has a nice Caffeine Database. I found it via a recent NYT article.
How To: Awake Fiberoptic Intubation
-
Printer Friendly|#| Trackback
This definitely falls in the "don't try this at home" category, but if this technique is different than the one you use, give it a try. It will surely result in a net gain in style points.
How To Do An Awake Fiberoptic Intubation
Technorati Tags: Anesthesia
More on pre-emptive positioning
-
Printer Friendly|#| Trackback
A fellow anesthesiologist wrote a reply to my post about pre-emptive positioning with the following:
"We've started doing the same thing at my surgicenter. At first I thought it was pretty ballsy when one of my colleagues suggested that we do simple one level laminectomies under LMA general and induce in the prone position. But now that we've started it I am very comfortable with the idea."
I'm not ready to try this yet (do you want to be my first patient?). Lateral or semi-sitting to supine is a matter of seconds. Prone to supine would take significantly longer I believe. Other experiences?
You Anesthesiologist Today Was...
-
Printer Friendly|#| Trackback
I finally ordered my own business cards. I've had generic one available but always had to write in my own name (despite being with the group for well over two years) so decided it was time for an upgrade.
Picking the pattern was tough, but I decided on a tranquil image (that happens to be one of the MacOS X desktop images):
Rejected images included a dark tunnel with a light at the end, and anything with pearly gates.
This decision was evidence based (of course). Giving patients a business card before anesthesia increases their recall of your name to about 50% rather than the 10% that remember it without. It should also help them see they are being cared for by a physician. There's room on the back for 'anesthetic' and 'comments', too.